Sentinel Lymph Node Biopsy in Breast Cancer: A Safe Step Towards Precision
For patients diagnosed with breast cancer, one of the most important steps is to find out whether the cancer has spread beyond the breast. Traditionally, this was checked by removing many lymph nodes from the armpit (axillary lymph node dissection). While effective, that method often led to long-term side effects like swelling of the arm (lymphedema).
Today, with medical advancements, a simpler and safer technique called Sentinel Lymph Node Biopsy (SLNB) has become the gold standard in breast cancer surgery.
What Is Sentinel Lymph Node Biopsy?
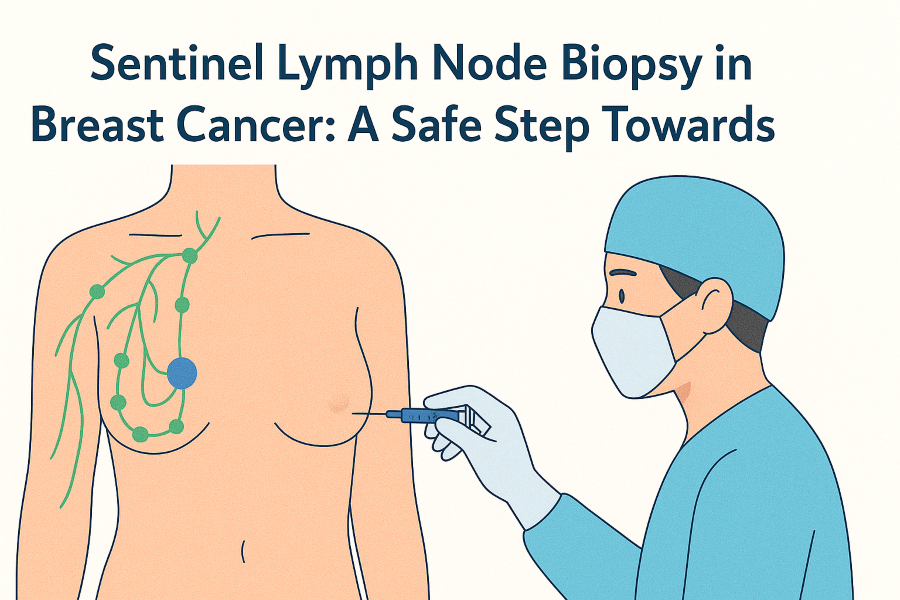
The sentinel lymph nodes are the first lymph nodes that receive drainage from the breast. If cancer spreads, it usually reaches these nodes first. By identifying and testing only these nodes, doctors can check whether cancer has spread—without removing all the lymph nodes.

This minimally invasive approach means less pain, fewer side effects, and faster recovery while still giving accurate staging information.
How Are the Sentinel Nodes Identified?
During the procedure, special dyes are used to highlight the sentinel lymph nodes:
- Methylene Blue Dye: A safe, widely used blue dye injected near the breast tumor or under the areola. It travels through lymphatic channels and stains the sentinel nodes blue.
- Indocyanine Green (ICG): A modern fluorescent dye that glows when viewed under near-infrared light, allowing surgeons to detect the sentinel nodes with high accuracy.
In many centers, both methods are used together to increase reliability.
How Is the Procedure Carried Out?
- Sentinel node biopsy is usually performed at the same time as breast surgery (lumpectomy or mastectomy).
- After injecting the dye, the surgeon tracks its path to identify 2–4 sentinel lymph nodes in the armpit.
- Only these nodes are removed and sent for microscopic examination.
- If cancer is not found in them, no further lymph node surgery is needed.

The procedure usually adds less than an hour to the overall surgery and does not prolong hospital stay.
Risks of Sentinel Node Biopsy
Although SLNB is much safer than full lymph node removal, some risks exist:
- Rare allergic reactions to the dye.
- Seroma (temporary fluid collection).
- Numbness or tingling in the arm.
- Very low chance of lymphedema compared to axillary dissection.
Benefits of Sentinel Node Biopsy
- ✅ Accurate staging of breast cancer.
- ✅ Minimally invasive with fewer nodes removed.
- ✅ Lower risk of lymphedema and arm stiffness.
- ✅ Faster recovery and shorter hospital stay.
- ✅ Better quality of life after surgery.
- ✅ Guides further treatment decisions like chemotherapy or radiation.
Frequently Asked Questions (FAQs)
1. Is sentinel node biopsy painful?
The procedure is performed under anesthesia during breast surgery, so you will not feel pain. Some mild discomfort at the incision site may occur afterward, but it usually improves quickly.
2. How long is recovery after sentinel node biopsy?
Most patients recover within a week. Normal arm movement and daily activities can be resumed faster compared to full lymph node removal.
3. Does everyone with breast cancer need sentinel node biopsy?
SLNB is recommended for most early-stage breast cancer patients. Your surgeon will decide if it is necessary based on your diagnosis.
4. Is there a risk of lymphedema after sentinel node biopsy?
The risk is very low (less than 5%), especially compared to axillary dissection where the risk is much higher.
5. Which is better—Methylene Blue or ICG?
Both are effective. Many cancer centers use them together for higher accuracy. ICG is considered more advanced due to its precision with fluorescence technology.
A Final Word
Sentinel lymph node biopsy is a safe, reliable, and patient-friendly procedure that has transformed the way breast cancer is treated. By focusing only on the most important lymph nodes, it provides accurate staging while protecting patients from unnecessary complications.
If you or your loved one is preparing for breast cancer surgery, speak to your doctor about SLNB. This small step can make a big difference in recovery, comfort, and long-term quality of life.